Singapore Nipped Things in the Bud
Germany Struggled with Delays
As has been widely reported, a novel coronavirus appeared in Wuhan, China in December 2019. Spreading rapidly through the city, and eventually the province of Hubei in January, countries and cities in the region started to implement travel restrictions in regards to Wuhan and eventually all of China. However, before its extremely infectious nature was known, many people from Wuhan and other parts of China had travelled across the globe. Singapore, fairly close geographically and economically to China, was one of the first countries to experience infections. From 20 January 2020, a business conference at the Hyatt hotel attended by many people from overseas, became one source of the spread of the virus to other countries, both in the region and globally. By mid-February, the numbers of infected persons in Singapore had reached over 70, which was at the time the second highest number of SARS-CoV-2 infected people worldwide after China. On 11 March 2020, the WHO declared the COVID-19 outbreak a pandemic, the first pandemic since the H1N1 Swine Flu in 2009. Now, by the end of April, in Germany, the number of infected people has well over-taken most of the countries in Asia, where it first circulated. In Singapore, although the number has also increased, it has been much more modest, at least until the mid of April. Indeed, the WHO has praised Singapore’s actions to contain COVID-19 infections. The WHO’s Chief, Tedros Adhanom Ghebreyesus, said in a press briefing on 10 March 2020, “Singapore is a good example of an all-of-government approach” (Aldgra 2020).
In the following, we comment and reflect on the different handling of COVID-19 in Germany and Singapore. We focus especially on the early phase of the pandemic in February and March. The daily current developments now, by the end of April, are difficult to comment on since it is almost impossible to read and reflect on the vast amount of daily published news and statistics in a comprehensive way. This will be the task of the future when the pandemic has been overcome to analyze and compare. Our preliminary conclusion is that Singapore has experienced epidemics previously and thus reacted more experienced, quickly and drastically to it than Germany. In Germany, studies and recommendations for handling the outbreak of a pandemic were available, amongst others the national pandemic strategy (Nationaler Pandemieplan) by the Robert-Koch-Institute of 2017. Nevertheless, in the initial phase of Covid-19, the recommended measures have not lead to a rapid emergency strategy in Germany.
Political deficiencies and cut backs to medical health systems in Germany
On 27 January 2020, at about the same time of the first COVID-19 case in Singapore, a case was also confirmed near Munich, Bavaria in Germany. The man who tested positive was an employee of a German car parts supplier who had contact with a Chinese colleague, who himself had had contact with people from Wuhan. According to Reuters, the infected persons were tested, monitored and isolated quite quickly (Poltz & Carrel 2020). The situation however was different in other regions. The Tyrolean ski resort town of Ischgl in Austria is accused of being a major coronavirus hotspot and the responsible persons such as owners of restaurants and the local authorities might be served a class action lawsuit (Schmidt 2020). From late February onwards, it had been clear that people were infected – amongst them one bar keeper of a highly frequented bar was tested positive – but they continued working in the restaurant for several days. The political authorities did not take action but kept the business going while discussing criteria on the appraisal of the COVID-19 risk and related protection measures. By the beginning of March, people who returned to Germany from skiing holidays in Ischgl were asked to serve a two weeks quarantine at home. Only on 13 March 2020, the Tyrolean authorities placed the entire town under quarantine.
Also in Germany, officials initially reacted very hesitant to the COVID-19 threat. Thereby, they revealed the fact that the warnings e.g. of World Health Organization (WHO) after the Ebola crisis in 2014-2016 and of the Robert-Koch-Institute to prepare for global virus pandemics had been a voice crying in the wilderness for the German healthcare system. In particular, political and medical authorities lacked adequate and rapid emergency strategies in response to the massive spread of COVID-19. In mid-March in Germany people were still not tested although they showed symptoms of heavy influenza and they themselves were asking to be tested. The reasons given by doctors and the public health authorities were that the ill persons had not had contact with a SARS-CoV-2 infected person and that they had not recently visited a high-risk region. An individual had to prove a substantial reason before getting tested (Blome 2020). Preventive examinations as a fundamental measurement for the handling and control of a virus pandemic obviously was an alien strategy for German authorities. An important reason was apparently the lack of available tests and related laboratories to handle these tests. In contrast to other European states, Germany might be celebrated as a role model case for managing the COVID-19 crisis due to the relatively low numbers of COVID-related deaths. However, Germany doesn’t look too well compared to some Asian states such as South Korea or Singapore where the policy of testing, tracing and treating decelerated the number SARS-CoV-2 infected people and prevented or at least postponed lockdowns.
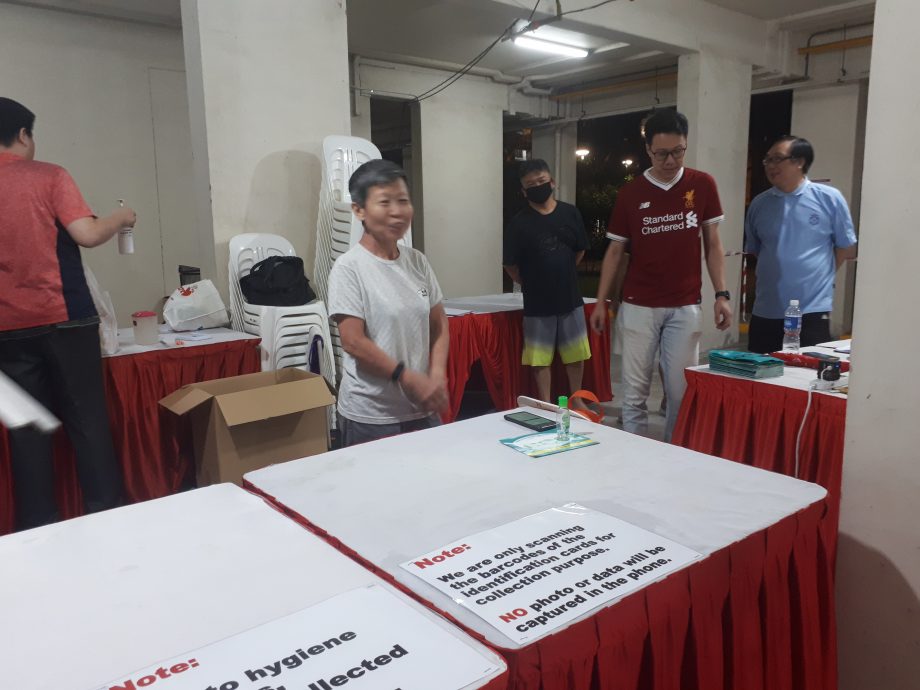
“Void desk” at a neighborhood distribution centre in Singapore where Singaporeans and permanent residents can fetch their masks (Photo by Maribeth Erb)
Fast reaction in Singapore
In contrast to Germany, it seems that Singapore reacted much faster and stricter to organize the fight against COVID-19. Even before the first infection was confirmed on 23 January 2020, on 2 January 2020, the Ministry of Health implemented temperature checks for passengers arriving at the international airport in Singapore from the Chinese province of Wuhan. Some days after the first case was confirmed, flights to Wuhan were cancelled, border control measurements were enhanced and people were asked to monitor their health. Singapore had experience with SARS in 2002, which is still fresh in many people’s memories until today. The thermal screening at airports developed during the SARS epidemic was quickly brought back in mid-January to monitor passengers coming in from China for temperature checks. So within the month, temperatures were being taken at many other places, particularly hospitals, and people had to make travel declarations, stating before they entered into hospitals and increasingly other public enclosed spaces, whether they had been to places with virus outbreaks (Min & Mohan 2020). At the National University of Singapore (NUS) in the beginning of February, employees had to take their temperatures twice a day and log it into a system. Lecturers were already being asked to migrate to online forms of teaching if their classes were above 50 students. Temperature taking and e-learning were measures developed during and in the wake of the SARS virus epidemic in Singapore. Thus, the SARS measures were something quickly brought to bear in response to COVID-19, and no one has blinked an eye about this (Youjin & Chandra 2020). For infected people, the Singapore government has been subsidizing expenses concerning the quarantine measures such as for food and medical supplies. Since end of March, all people returning to Singapore from abroad were brought directly to hotels to serve out their stay-at-home notices, instead of going home to potentially infect family or other household members. Again, these measures have been subsidized or entirely paid for by the government, depending on the region of the world travelers were returning from. From the very beginning, everyone identified with COVID-19, even if they weren’t very sick, were brought to the National Centre for Infectious Diseases for isolation, and anyone who had been in contact with them was also isolated. The strategy to isolate infected persons is different from Germany, where people are told to stay home (with their family) if they are not very ill. We believe this is one of the reasons Singapore has managed to keep some control over the virus in beginning. Currently, those who are clinically well but still testing positive, are moved out of the hospitals dedicated to the care of COVID-19 patients, and moved either to other hospitals, or to other spaces of isolation where they are cared for until they test negative.
Unfortunately, due to many imported cases, mostly returning residents from other countries where infections were becoming rampant, the numbers of cases in Singapore has been on the rise since mid-March. Unlike many other countries, Singapore had not been on any kind of “lockdown” through the months of February and March, despite the long known presence of the disease on its shores. With preventive measures in place, most people continued to go about their normal life. However, with the rise in cases over the last week of March and early April, the Singapore government has felt that more stringent measures are needed. This has also been the experience of other countries in Asia which had a quick response, such as Hong Kong, where the initially small numbers of infections started to rise rapidly with the return of people from Hong Kong, such as exchange students, from other parts of the world seriously affected by COVID-19 (Graham-Harrison 2020).
In Singapore, beginning 7 April 2020, a lockdown has started, with all non-essential stores being shut down, and non-essential service employees being asked to work from home. Also beginning 7 April 2020, the authorities have started monitoring public spaces to make sure that people are not congregating and primarily staying at home, practices that have been in place in Germany for weeks now.

Neighborhood hawker centre Singapore 7 April 2020 (Photo by Maribeth Erb)

Neighborhood hawker centre Singapore 6 April 2020 (Photo by Maribeth Erb)
An unfortunate development in Singapore, which has seen an explosion of infections after the beginning of what the government calls a “circuit breaker”, is the tremendous surge in cases among the migrant worker community. Foreign workers, hired mostly to work in construction and estate maintenance, considered essential industries, are housed in dormitories where they are in close contact both in their residences and during work. Outbreaks among the numerous dormitories have seen hundreds of new cases identified every day. The government has taken pro-active measures to test these workers, isolating and treating those affected, and separating those still well to contain this newest source of the outbreak in Singapore. The Singapore government has apparently put aside the embarrassment of admitting a huge rise in the number of cases, to make sure that the infections can eventually be brought under control.
Conclusion
The COVID-19 crisis is a global danger to health, which in the whole world has resulted in radical changes in social behaviour, economic adjustments and roles of governments. Yet, the above examples of Germany and Singapore show that regional responses have been very different. Whereas Singapore has based its measures on previous experiences with the SARS epidemic in 2002, Germany seemed to be struggling in their response to the pandemic crisis, and this tragically has been the case in many other parts of the world as well. Surely, measurements that are implemented in Singapore cannot be transferred one to one to Germany or other countries. Different political and medical systems, diverse experiences and approaches to illness and pandemics lead to different handlings. However, it is to be hoped that the reflections on these different experiences will lead to the awareness of the need for a pandemic emergency plan, globally and locally, which can take early action.
Written on 2 April 2020 / final submission on 21 April 2020
Kristina Großmann is an Assistant Professor at the Chair of Comparative Development and Cultural Studies with a Focus on Southeast Asia at the University of Passau, Germany. In February 2020 she cancelled her flight to Singapore because of COVID-19 and since then has been discussing this issue vibrantly with her German and Southeast Asian colleagues.
Maribeth Erb is an Associate Professor at the Department of Sociology at the National University of Singapore (NUS). Originally from the US, She has worked and lived in Singapore since 1989.
Nicole Weydmann is Postdoctoral Researcher at Jacobs University in Bremen and works on traditional and alternative medicine in Southeast Asia and Europe.
Novia Tirta Rahayu Tijaja completed her MA degree in Southeast Asian Studies at the University of Passau and currently stays in her hometown Jakarta.
#WitnessingCorona
This article was simultaneously published on the Blog Medical Anthropology. Witnessing Corona is a joint blog series by the Blog Medical Anthropology / Medizinethnologie, Curare: Journal of Medical Anthropology, the Global South Studies Center Cologne, and boasblogs.
Bibliography
Aldgra, F. 2020. WHO refused to acknowledge Taiwan, praises Singapore instead. https://www.theonlinecitizen.com/2020/03/30/who-refused-to-acknowledge-taiwan-praises-singapore-instead/. Last access: 17/04/2020.
Bloome, Rebecca. 2002. Momentaufnahme: Überlastete Covid-19-Untersuchungsstellen und die Koordination von Verdachtsfällen in Berlin (#WitnessingCorona) https://boasblogs.org/witnessingcorona/momentaufnahme/ & https://www.medizinethnologie.net/ueberlastete-covid-19-untersuchungsstellen/
Last access: 17/04/2020
Graham-Harrison, Emma. 2020. Coronavirus: how Asian countries acted while the west dithered. https://www.theguardian.com/world/2020/mar/21/coronavirus-asia-acted-west-dithered-hong-kong-taiwan-europe. Last access: 17/04/2020.
Min, Ang Hwee & Mohan, Matthew. 2020. One month of COVID-19: Concern, containment and collective effort. https://www.channelnewsasia.com/news/singapore/covid19-singapore-one-month-coronavirus-containment-12454450. Last access: 17/04/2020
Poltz, Jörn & Carrel, Paul. 2020. Pass the salt: The minute details that helped Germany build virus defences. https://www.reuters.com/article/us-health-coronavirus-germany-defences-i/pass-the-salt-the-minute-details-that-helped-germany-build-virus-defences-idUSKCN21R1DB. Last access: 17/04/2020.
Robert Koch Institut. 2017. Nationaler Pandemieplan Teil I. Strukturen und Maßnahmen
Stand: 2. März 2017. https://www.gmkonline.de/documents/pandemieplan_teil-i_1510042222_1585228735.pdf. Last access: 17/04/2020
Schmidt, Nadine. 2020. Austrian officials face lawsuit from 2,500 tourists over ski resort outbreak. https://edition.cnn.com/travel/article/austria-ski-resort-ischgl-coronavirus-intl/index.html. Last access 17/04/2020.
Youjin, Low & Chandra, Alif. 2020. The Big Read: Panic buying grabbed the headlines, but a quiet resilience is seeing Singaporeans through COVID-19 outbreak. https://www.channelnewsasia.com/news/singapore/coronavirus-covid-19-panic-buying-singapore-dorscon-orange-12439480. Last access 17/04/2020.